Shingles is a viral infection that is characterized by painful blisters and skin lesions. It is seen to be more common in adults and more so in the case of males as compared to females.
Shingles is initially characterized by the onset of fever, malaise, unilateral pain and tenderness along the course of nerves. It later leads to vesicular type of painful rashes along the course of the affected nerves. These are usually fluid filled vesicles that may rupture in due course of time for the commencement of healing. There may also be tingling, itching or prickling type of sensation in the affected nerves or rashes.

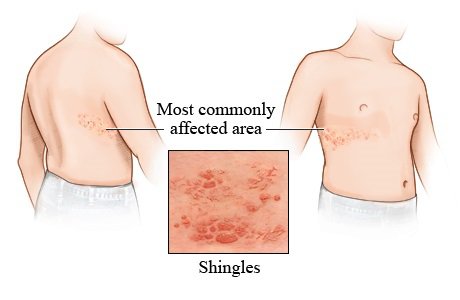
Shingles generally affects one side of the torso of the body, the regions around the eyes, or the sides of the neck and the face. Sometimes, the infection may go unnoticed as there is no appearance of blisters, but there is only the pain that can be felt. In such cases, diagnosis of the disease becomes difficult as the pain may be mistaken to be caused by something else.
Sometimes, even after the normal course of the infection, which is typically in between two weeks to six weeks, the pain can still be experienced. This is because the infection is a nerve infection which may prove to damage the nerves. In such cases, damaged nerves tend to send out false signals and also greatly exaggerated signals of pain being experienced, even when the infection may have long subsided.
Shingles is not a life threatening condition and typically, the painful conditions and symptoms of Shingles disappear on their own after the duration of the course of the infection is over [1]. Typically, the duration of an episode of Shingles infection can last for anything in between two weeks to six weeks. An early diagnosis of the signs and symptoms of Shingles may help in achieving a speedier recovery. Most people only face a single episode of Shingles in their entire lifetime but in some cases in which the immunity of the body is greatly lowered, individuals may experience multiple outbreaks of the virus and multiple episodes of Shingles. Nevertheless, it is still extremely rare to experience more than three outbreaks of the disease.
Causes of Shingles – The Varicella Zoster Virus
Shingles, also known as Zona is caused by the chickenpox causing Varicella Zoster virus. The virus is a double stranded DNA virus that leads to development of the painful condition. While the Varicella Zoster virus is similar to the Herpes Simplex Virus and both belong to the same family, they prove to have different actions and cause different signs and symptoms in individuals. There is usually differential diagnosis between the two types of virus. Even though both the virus types belong to the herpes family, The Varicella Zoster virus does not cause herpes or other transmitted diseases such as cold sores.
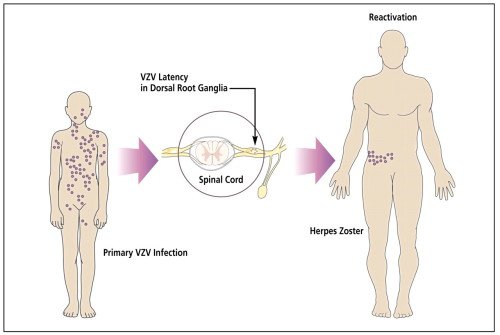
Varicella Zoster virus is the virus which also causes chickenpox [2]. If an individual encounters an episode of chickenpox in his lifetime, even after the disease has long been treated and forgotten about, the virus remains dormant in some parts of the body, especially the dorsal root ganglia cells present in the spinal cord and in the brain. If the dormant virus is reactivated due to some external or internal trigger, then Shingles will be developed by the individual.
While it is well known that it is the same Varicella Zoster virus which causes both chickenpox and Shingles, the exact triggers as to what causes the reactivation of the dormant virus still remains largely unknown. However, it can also be seen that the risk of encountering Shingles is greater as an individual ages or in those undergoing cancer treatment, leading to the widely agreed upon belief that a weakening of the immune system can be linked to the conditions of reactivation of the dormant virus.
Blisters caused by Shingles are typically only confined to one side of the body and are grouped into clusters in stripes. While they typically manifest on one side of the torso or the waistline, they may also infect one side of the face, one side of the neck, or even the region around one eye. In such cases, special care must be taken as the blisters may easily damage the optical nerve, leading to permanent eye damage and even loss of vision.
Mechanism of action of Zoster Virus
The Varicella Zoster virus is present in a dormant or inactivated form in the bodies of those individuals who have experienced an episode of chickenpox at some point of time in their lives and also those individuals who have been injected with Varicella vaccine. The Varicella Zoster virus remains inactive in the dorsal root ganglia cells and other nerve cells without causing any noticeable effects in the body until it is reactivated by an external or internal stimulus [3]. While the immune system of a normal individual proves to suppress the reactivation of the virus, individuals in whom the immune system is weakened or compromised may suffer from reactivation of the dormant virus.
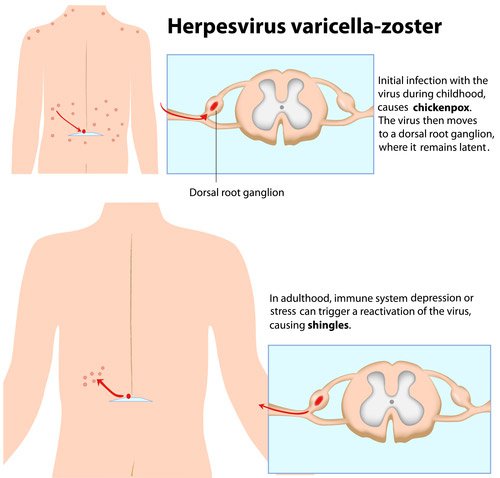
The reactivation of the Varicella Zoster virus leads to inflammation of the dorsal root ganglia, after which the virus multiples and spreads by travelling along the course of nerves to the superficial nerves of the body, ultimately reaching the surface of the skin. On reaching the superficial nerves, they further lead to the development of painful rashes and blisters in form of stripes.
These blisters are both itchy and painful and contain fluids which ooze out over the course of time. Medical examination has revealed that the blisters also contain the Varicella Zoster virus. Thus the virus, which had once affected an individual early on in life, remains dormant for a lengthy course of time until reactivated. As soon as it is reactivated, the virus multiplies at great speeds and spreads to the surface of the skin from where on it may prove to be transmitted contagiously on to another person.
Risk factors for Shingles
Individuals may encounter chickenpox and Shingles at any point of time in life. While chickenpox is more closely associated with childhood and early adulthood, Shingles is associated with elderly age, even though the same virus is what causes both of these diseases.
Once an individual has encountered chickenpox, even the mildest form of the infection, or once an individual has been vaccinated using the Varicella vaccine, the virus comes to find a presence in the individual’s body. While this virus is more so in a dormant form, it may be triggered or activated.
Herpes Zoster or Shingles is caused by the reactivation of Varicella virus due to a number of factors [4]:
- Immune-suppressive drug therapy: An individual’s body suppresses the Varicella virus in a normal case, thus preventing the reactivation of the virus. However, the lack of proper immunity in the case of immune-compromised individuals, may lead to reactivation and also outbreak of the virus in a much more vigorous form. It is often seen that the use of drugs such as corticosteroids may lead to immune system suppression.
- Ageing: With ageing, the immunity of an individual may be lowered and may help Varicella to break from the dormant phase. Studies have also revealed that many experts believe that after the age of 80, half of the total number of people will encounter Shingles.
- Psychological stress: Stress is another major cause for suppressing the immunity leading to activity of virus again. It is recommended to always keep the body healthy and to keep stress levels in check in order to avoid an outbreak of the Varicella virus.
- Medical conditions like HIV or cancer: Any malignancies or HIV infections may also adversely affect the immune system by lowering the count of white blood defense cells in the body. It is often the case that patients who are diagnosed with cancer and are undergoing therapy may face an episode of Shingles.
- Radiotherapy: Radiation therapy is another major cause for lowering the immunity. Alongside chemotherapy, Shingles is most commonly encountered by cancer patients undergoing radiation therapy.
- Stress: Acute trauma or stress may also prove to give a sudden shock to the immune system and may lead to the reactivation of the dormant Varicella virus.
- Pregnant Women: Pregnant women are also at a higher risk of encountering the disease. Even if the condition is mild, if encountered, Shingles can affect the normal development of the baby as well.
- Medications: Certain medications which are prescribed after an individual has undergone an organ transplant so that the body does not reject the foreign organ require suppressing the immune system by a great deal. In such conditions, the risk of encountering Shingles is quite high.
- Family History: It is often the case that an individual who has experienced an episode of Shingles will have many other family members who have also encountered the disease.
- Bone Marrow Transplants: Bone marrow transplants leave the state of the immune system of the body highly weakened and defenseless. Individuals who have recently undergone a transplant surgery are at a high risk of developing Shingles.
Anybody who has encountered even the mildest of chickenpox infections is at a risk to developing Shingles. However, even those people who have been injected with the Varicella vaccine have the virus present in their body and as such, are also at a higher risk to encountering the condition than a normal individual who has never been vaccinated or has suffered from chickenpox.
While the exact mechanism of how the virus is reactivated from its dormant state and what actually proves to be the trigger, external or internal is still far from being understood, the risk factors of the causes of Shingles are generally widely agreed upon.
If an individual is suspected to be facing a risk factor to encountering Shingles, proper medical consultation must be sought at the earliest. An early diagnosis may lead to a speedier recovery and will also prevent the chances of complications. While there is no real treatment method for Shingles, there are many medications which can help prevent the virus from spreading and many others help in alleviating the pain associated with the blisters.
Transmission of Shingles
Shingles is a contagious disease and it may spread to other individuals through direct body contact through the fluid filled blisters or the unhealed sores and wounds where scab is yet to form. It is more prone to be transmitted to people who are low on immunity. It is always advised to keep the blisters covered and to avoid contact when suffering from the condition.
Shingles is considered to be contagious only during the active phase of the blisters. This means that before the appearance of blisters and after the drying up of the sores on the surface of the skin, Shingles cannot be transmitted contagiously.
Shingles cannot be transmitted by sneezing, coughing or through the air [5]. Direct body contact with the fluid coming out of the oozing sores is what can cause the virus to be transmitted to another individual.
A person who has been vaccinated against chickenpox or one who has encountered chickenpox earlier in life cannot develop Shingles through transmission by body contact.
If an individual is not vaccinated against chickenpox and Shingles, it must be done at the earliest in order to prevent encountering the contagious disease.
Preventing the Varicella Zoster Virus from spreading
Utmost care must be taken to avoid the highly contagious virus from spreading. Anybody suffering from Shingles should make sure never to share clothes or towels with other individuals, should avoid swimming in public areas and also should avoid playing any sports which involve contact.
In case there is oozing from the rashes and blisters and fluid comes out of the skin lesions, it is recommended to take the day off and to abstain from school or work.
It is always advised to cover all the blisters and rashes if meeting other individuals so as to prevent the virus from spreading. While the condition can be really painful and irritating, sufferers will also need to maintain care from their end so as to prevent spreading the virus to other individuals.
Reference
[1] Journal of Crohn’s and Colitis: Second European evidence-based consensus on the prevention, diagnosis and management of opportunistic infections in inflammatory bowel disease,, Rahier, J. F., Magro, F., Abreu, C., Armuzzi, A., Ben-Horin, S., Chowers, Y., & Colombel, J. F.: Volume 8 Issue 6. Pp. 443-468 – June 2014 – DOI: http://dx.doi.org/10.1016/j.crohns.2013.12.013, http://ecco-jcc.oxfordjournals.org/content/8/6/443.extract
[2] Journal of virology: Global Identification of Three Major Genotypes of Varicella-Zoster Virus: Longitudinal Clustering and Strategies for Genotyping, Loparev, V. N., Gonzalez, A., Deleon-Carnes, M., Tipples, G., Fickenscher, H., Torfason, E. G., & Schmid, D. S. ; Volume 78 Issue 15. Pp. 8349-8358 – August 2014 – doi: 10.1128/JVI.78.15.8349-8358.2004 http://jvi.asm.org/content/78/15/8349.short
[3] Clinical Infectious Diseases: Recommendations for the Management of Herpes Zoster, Dworkin, R. H., Johnson, R. W., Breuer, J., Gnann, J. W., Levin, M. J., Backonja, M., … & Whitley, R. J. ; Volume 44 Issue Supplement 1. Pp. S1-S26 – July 2007 – doi: 10.1086/510206 http://cid.oxfordjournals.org/content/44/Supplement_1/S1.short
[4] The Journal of Infectious diseases: Varicella-Zoster Virus: Atypical Presentations and Unusual Complications, Gnann, J. W.; Volume 186, Issue Supplement 1. Pp. S91- S98 – September 2002 – doi: 1086/342963 http://jid.oxfordjournals.org/content/186/Supplement_1/S91.short
[5] Mathematical Model of Natural Phenomena: A Cost-Effectiveness-Assessing Model of Vaccination for Varicella and Zoster, Comba, M., Martorano-Raimundo, S., & Venturino, E.; Volume 7 Issue 3. Pp. 62-67. – January 2012- DOI: http://dx.doi.org/10.1051/mmnp/20127306
