Shingles is an acute viral infection that is characterized by the appearance of rashes or blisters on the body which also prove to be quite painful. While these rashes can appear at any part of the body, it is most commonly characterized by stripes of blisters around the sides of the torso. The rashes and blisters associated with Shingles are caused by an inflammation of the nerves located underneath the surface of the skin.

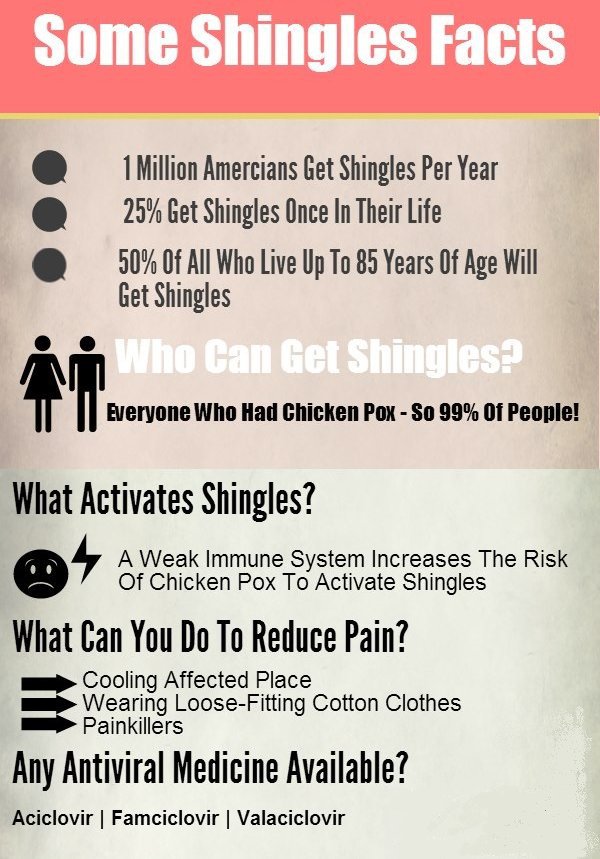
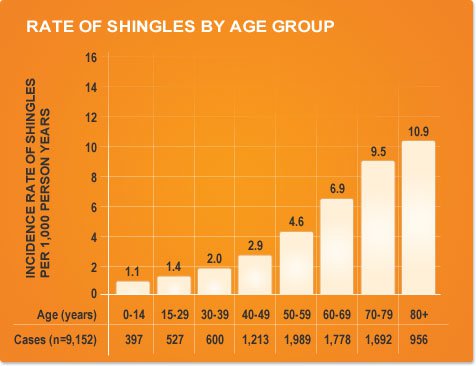
Shingles also goes by the names of Zona and of Herpes Zoster and is caused due to the reactivation of the Varicella Zoster virus in the body of an individual who has suffered from chickenpox in the past [1]. It is estimated that every 1.2 to 3.4 out of every thousand individuals suffers from Shingles worldwide. In US, the incidence rate of the infection is 3.1-3.2 per 1000 individuals.
Shingles may not be a life threatening condition, but it definitely proves to be really painful and uncomfortable. Early diagnosis can lead to quicker treatment and shorten the course of the infection. Today, there are also a number of vaccines available in the market which can help prevent the infectious disease.
Causes of Shingles
The primary cause for Shingles is the presence of the Varicella Zoster virus in a dormant or inactivated form [2]. The virus is present in the bodies of individuals who have experienced an episode of chickenpox in their lives or individuals who have been injected with the varicella vaccine. This Varicella Zoster virus remains inactive in the dorsal root ganglia present in either the spinal cord or in the brain in the host’s body until it is reactivated by either an external or an internal stimulus. This reactivation leads to inflammation of these ganglia and further develops into painful rashes and blisters over the body, most commonly in the form of stripes.
Shingles is observed to occur more commonly in elderly individuals and as such, its cause is also linked to a weakened immune system. What exactly triggers the reactivation of the virus is still unknown.
While the Varicella Zoster virus belongs to the herpes family of virus, the specific virus which causes Shingles and chickenpox is different from that which causes herpes or cold sores.
There are a number of risk factors to developing Shingles – the foremost of them being individuals who have suffered from chickenpox at some point of time in their lives. Even apart from these individuals, others may be at a risk of encountering the infectious disease in case of the following:
- If the individual is over 50 years old, the risk of encountering the disease is much higher due to a weakened immune system. It is also estimated by some experts that over half the total number of people above the age of 80 will develop Shingles.
- If individuals suffer from cancer or HIV AIDS, the immune system is greatly weakened and Shingles may easily be encountered.
- Individuals undergoing therapy for cancer such as chemotherapy or radiation therapy are also at a higher risk of encountering Shingles as the body resistance to infections is greatly lowered.
Certain medications which are prescribed to prevent the chances of rejection of newly transplanted organs in the body can also prove to increase the risk of individuals encountering Shingles. Prolonged usage of some steroids such as prednisone can also prove to increase the risk factor.
Signs and Symptoms of Shingles
Shingles occurs more commonly in males than in females and more so in adults. The rash caused by Shingles is much more common on the body, but it can also happen on the face and in eyes. Shingles rash can also affect pregnant women.
Usually, the first and the foremost symptom to be associated with Shingles is the development of unexpected pain. There have been many cases in which pain is the only symptom in individuals and there is no appearance of any rashes.
Shingles usually manifests in the form of a stripe of rashes or blisters which appears on the sides of the torso. The rash may also occur on the sides of the neck, on the face and around the eyes.
The common signs and symptoms of Shingles include:
- Initially, the condition is characterized by fever, malaise, pain and tenderness along the course of nerves. The pain is usually unilateral, that is it occurs in one half of the body.
- The initial pain later develops into vesicular type of painful rashes along the course of the affected nerves. These fluid filled vesicles may rupture in due course of time for the commencement of healing.
- Vesicles are extremely painful and incapacitating due to involvement of nerves. Burning, stabbing or excruciating pain is often what is described for this condition’s symptoms.
- There may also be tingling, itching or prickling sensations in the affected nerves or rashes.
- The vesicles may also get infected by other secondary infectious agents thus proving to interfere with the natural course of healing.
- Herpes zoster may also affect the nerves of face leading to painful vesicles in the oral cavity including tongue, larynx, pharynx etc.

In case the signs and symptoms of Shingles are suspected, it is recommended to seek medical attention at the earliest [4]. Attention should be provided immediately in case of the following;
- If the rash and the pain is being experienced around the eyes. If left untreated, the infection can also cause permanent damage to the eyes.
- If an individual has a weakened immune system or has a history of family members having weak immune systems. This may be due to chronic illnesses, medications or even other diseases such as cancer.
- If the individual in over 70 years of age, the chances of complications due to the rashes is significantly higher. As such, immediate medical attention needs to be provided in order to keep complications at bay.
- Immediate medical attention should always be provided in case the rashes are widespread on the body and also painful.
Shingles – The causes, symptoms, treatment and prevention
Is Shingles contagious?
Yes, Shingles is a contagious disease. A person suffering from Shingles may easily infect another individual with the Varicella Zoster virus [3]. Typically, the virus is transmitted on bodily contact involving the sores and wounds of the rash.
When a person is infected from another, the development of chickenpox is a certainty even if Shingles is not developed.
The following types of individuals are the most prone to being infected contagiously from Shingles sufferers:
- Individuals who have a weakened immune system
- Newborns and infants
- Women undergoing pregnancy
Is Shingles painful?
Shingles is accompanied by a sharp and severe pain, often much greater than what people anticipate it to be. While the vesicles or rashes that occur in Shingles are extremely painful and also incapacitating due to the involvement of nerves, there are also many cases in which individuals experience pain without the appearance of any lesions on the surface of the skin. In such cases, the pain may be mistaken to be originating due to some other cause such as appendicitis, headaches, abdominal pains, sciatica and also heart attacks.
The pain associated with Shingles is very severe and is often so unbearable that sufferers cannot even sleep during the active blister phase. This sharp pain may sometimes even persist even after the subsiding of blisters. This happens in case the nerves are damaged during the infection and they subsequently send out false or exaggerated signals of pain.
The painful condition associated with Shingles can only be relieved with the help of certain anesthetic blocks or pain killer drugs and that too, only temporarily.

It is recommended to take baths with cold water and also to apply cool and moist wipe cloths on the rashes throughout the duration of the infection in order to relieve itching or pain. Baking soda can also help the blisters and sores to dry off and heal quicker. The sores should be soaked with tap water to clean away any crusts and also to decrease the oozing. Proper care needs to be taken of the blisters so as to relieve the painful and the irritating symptoms.
Some of the over the counter pain medications such as aspirin, ibuprofen and acetaminophen can also help in reducing the symptoms of pain. However, it is important to always consult a professional medical expert in case prescription medication is being taken alongside these over the counter drugs.
Shingles Complications
If not properly attended to, Shingles can cause a number of other complications which may include:
- Skin problems: If not treated properly, the vesicles may become secondarily infected by bacteria and cause infection or diseases on the skin surface.
- Loss of vision: In case of shingles around the eyes, inflammation of the ophthalmic nerve (the nerve which supplies blood to the eye) might occur, which may consequently lead to infection and ultimately to a loss of vision.
- Postherpetic neuralgia: Inflammation of the nerve ganglion may leave the nerve fibers damaged which may cause pain even after subsiding of the shingles infection. This is because the damaged nerves send out greatly exaggerated signals of pain to the brain.
- Various neurological problems: There may be a number of neurological problems if shingles if left untreated. An example of this is the Ramsay-Hunt’s Syndrome, which involves an infection of both the mouth and the ear by the virus, leading to facial paralysis, hoarseness of voice, tinnitus, vertigo and many other bodily disturbances.
Shingles Diagnosis
The Shingles disease is usually diagnosed externally, based on the appearance of skin lesions, rashes and blisters or based on the history of pain occurring on one side of the body. In some cases, a culture of the skin tissue containing the blisters is also analyzed to confirm the disease.
Shingles is confirmed by microscopic examination of the smear collected from the infected sites. This test is commonly known as Tzanck test. It may also be diagnosed with viral culture testing in the lab.
Shingles Treatment
There is no particular medication or treatment of this infectious disease as it subsides on its own with time. Typically, the duration of the Shingles infection lasts in between two to six weeks. While the majority of individuals encounter the disease only once in their lifetimes, there are some cases of individuals having suffered more than a single episode of Shingles in their lifetimes.

There are antiviral drugs and medicines for Shingles, which can prevent the condition from worsening and can also prevent complications. Some examples of medications which are commonly prescribed for Shingles sufferers include the following:
- Zovirax, also known as Acyclovir
- Valtrex, also known as Valacyclovir
- Famvir, also known as Famciclovir
In case of severe pain, the following medications are also prescribed:
- Gabapentine and other anticonvulsants
- Capsaicin cream
- Codeine or other narcotics
- Amitriptyline and other tricyclic antidepressant drugs
- Local anesthetics or injections of corticosteroids
- Skin patches, sprays, gels and creams containing numbing agents such as lidocaine
Prevention and Vaccination of Shingles
There are some Shingles vaccines which can prevent the infection from occurring if taken on time [5]. The vaccines which are used include:
- Varivax: This is a vaccine for chickenpox and is widely administered. While this vaccine does not guarantee the prevention of shingles or chickenpox for that matter, the vaccine nevertheless greatly reduces the chances of any complications in case the disease is encountered as also the severity of the disease is greatly reduced.
- Zostavax: This vaccine has been approved for use by the FDA and helps fight Shingles infection. While the vaccine is not a guarantee against the disease, the likelihood of encountering Shingles is greatly reduced as also is the risk of complications and postherpetic neuralgia.

Shingles vaccines contain the live forms of the virus which cause chickenpox or Shingles. As such, they are to be used only as a preventive measure and should never be administered to individuals who are suffering from the disease conditions. People who are suspected to have weak immune systems should also not be administered vaccines.
References
[1] Antimicrobial Agents and Chemotherapy: Susceptibilities of Several Clinical Varicella-Zoster Virus (VZV) Isolates and Drug-Resistant VZV Strains to Bicyclic Furano Pyrimidine Nucleosides, Andrei, G., Sienaert, R., McGuigan, C., De Clercq, E., Balzarini, J., & Snoeck, R.; Volume 49 Issue 3. Pp. 1081-1086 – March 2005 – doi: 10.1128/AAC.49.3.1081-1086.2005 http://aac.asm.org/content/49/3/1081.short
[2] Journal of virology: Varicella-Zoster Virus Immediate-Early Protein ORF61 Abrogates the IRF3-Mediated Innate Immune Response through Degradation of Activated IRF3, Zhu, H., Zheng, C., Xing, J., Wang, S., Li, S., Lin, R., & Mossman, K. L. ; Volume 85 Issue 21. Pp. 11079-11089 – November 2011 – doi:10.1128/JVI.05098-11 http://jvi.asm.org/content/85/21/11079.short
[3] Cambridge Journals: Epidemiology and Infection, Pannell, R. S., Fleming, D. M., & Cross, K. W.; Volume 133 Issue 6. Pp. 985-991 – May 2005 – DOI: http://dx.doi.org/10.1017/S0950268805004425, http://journals.cambridge.org/action/displayAbstract?fromPage=online&aid=350197&fileId=S0950268805004425
[4] America Journal of Epidemiology: The Interval between Successive Cases of an Infectious Disease, Fine, P. E.; Volume 158 Issue 11 Pp. 1039-1047 – May 2003 – doi: 10.1093/aje/kwg251 http://aje.oxfordjournals.org/content/158/11/1039.short
[5] The New England Journal of Medicine: Varicella Vaccine and Infection with Varicella–Zoster Virus, Vázquez, M., & Shapiro, E. D. ; N Engl J Med 2005; 352. Pp. 439-440 – Feb 2005 – DOI: 10.1056/NEJMp048320 http://www.nejm.org/doi/full/10.1056/nejmp048320
